Building the Continuum of Care to Quell the COPD Epidemic
To address the COPD epidemic, healthcare payors and providers must create a continuum of care that supports proactively and continuously after diagnosis.
COPD, one of the leading causes of death around the world, is widely considered to be a preventable epidemic. But shortcomings in public policy and healthcare delivery leave millions of people behind—without access to timely specialist care, and often without an accurate diagnosis.
To address this escalating problem, healthcare payors and providers must create a continuum of care for COPD, starting with early diagnosis and following patients through the stages of this progressive disease.
The diagnostic shortfall and the impact of care gaps
COPD impacts over 25 million adults in the U.S., but studies suggest that up to 15 million more are living without a proper diagnosis. The prevalence of underdiagnosis is attributed to several interconnected factors, namely:
- A systemic shortage of diagnosis in primary care settings
- Shortages of pulmonology care
- Underutilization of spirometry
- Patients underreporting symptoms in early stages
Simply put, there are significant and systemic barriers to healthcare access that prevent patients from receiving a timely COPD diagnosis, especially among vulnerable populations like members of historically marginalized communities and those in rural areas. As a result, millions of people go without care as their disease progresses, accruing costly comorbidities as they age—and over 80% of COPD patients have at least one comorbidity. Consequently, comorbidities are shown to more than double hospitalization rates, resulting in more severe exacerbations, longer hospital stays, and ER readmissions. The result is almost $30 billion in direct healthcare costs and $20 billion lost in productivity.
Conversely, patients who do receive an early diagnosis were found to have “fewer exacerbations, fewer comorbidities, and lower health care utilization,” when compared to patients who received a late diagnosis. Thus, early detection and diagnosis are critical to managing COPD and mitigating its impact.
Achieving early and accurate diagnoses
Because the risk factors for COPD are complex and varied, including environmental exposure, genetic predisposition, and tobacco usage, risk profiles are also similarly complex. Overcoming the diagnostic shortfall demands solutions that can meet people where they are, with sufficient personalization to empower patients and providers to track and manage the disease over time.
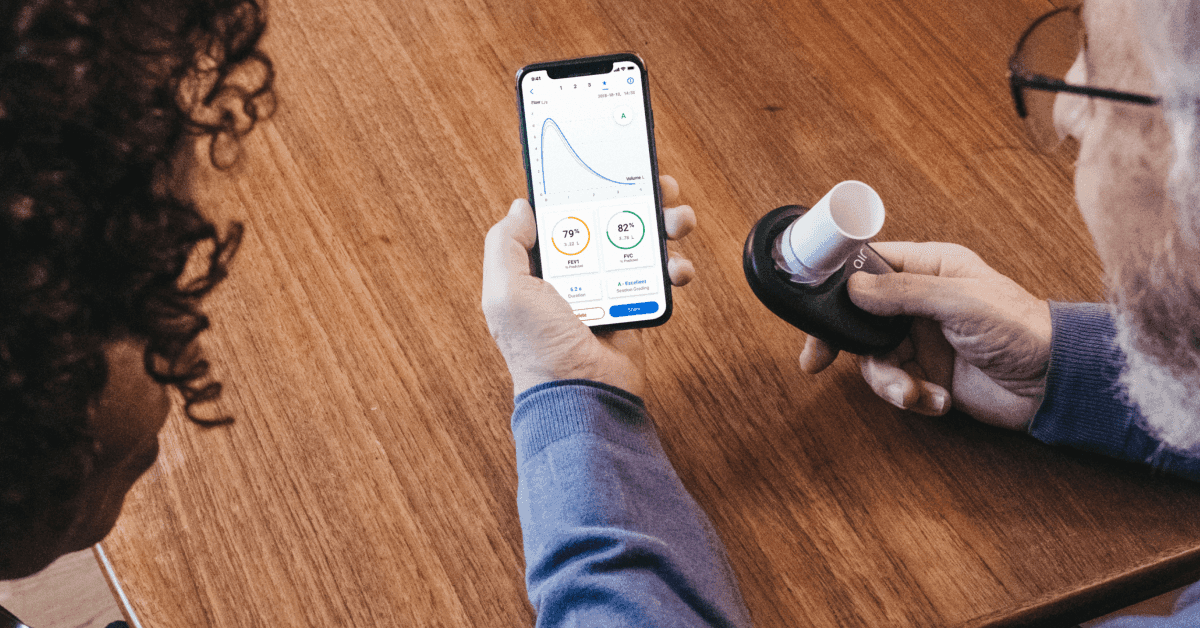
To achieve this, we must first expand access to diagnostic services through high-quality spirometry with solutions that are accessible at home and are easy to use. NuvoAir collaborates with partners like Signify Health to offer diagnostic services that leverage Bluetooth-enabled devices for their in-home care teams to diagnose COPD for at-risk individuals. After receiving or confirming a diagnosis, we can enroll patients in our ongoing clinical service to ensure they’re receiving continuous and proactive care. With increased scrutiny from CMS on risk adjustment and coding accuracy, it’s more important than ever for health plans and providers to ensure patients with high-risk adjustment factor (RAF) scores receive ongoing care for chronic diseases like COPD, lest their hard-fought diagnosis becomes what some healthcare executives refer to as an “orphan diagnosis.”
As care moves from facilities to the home, NuvoAir and its partners can overcome many barriers facing early and accurate diagnosis by empowering patients and providers with powerful technology and virtual clinical support. Patients don’t have to wait for symptoms to worsen to see a doctor, nor do they have to travel to an office where spirometry services may or may not be available. Likewise, because the Air Next spirometer from NuvoAir is easy-to-use, we can collect high-quality data in real-time for use in both diagnostic and ongoing care.
Expanding access to diagnostic services is only the first step. At NuvoAir we believe that patients need and deserve comprehensive and ongoing support as their disease progresses so that they can stay on top of their health and ahead of costly and dangerous exacerbations.
Comprehensive and personalized care for COPD
As a virtual-first specialty care provider, NuvoAir provides comprehensive and personalized care for patients with cardiopulmonary conditions. Together with our partners across the healthcare ecosystem, we facilitate a continuum of care for people with chronic heart and lung diseases so they can receive the ongoing care they need.
NuvoAir’s care model offers an integrated, end-to-end solution that conducts proactive, personalized clinical interventions to improve outcomes and reduce costs through tailored care programs that can prevent exacerbations by generating and evaluating clinically relevant data that’s actioned upon by a multidisciplinary virtual care team.
This data is ingested through our engagement engine which helps our care team detect exacerbations, adjust treatment plans, and execute relevant clinical interventions including pulmonary rehabilitation, smoking cessation, and more. Patients can access same-day appointments with our multidisciplinary care team through our virtual clinic, so they can get support whenever they need it, rather than potentially waiting for months for an in-person appointment.
“Through our care model, we capture and assess ongoing data, see signals, identify trouble spots, and intervene before the patient heads to an office visit or emergency room,” says Michael Zagami, Chief Product Officer at NuvoAir.
As a result, NuvoAir drives positive outcomes and lower costs for people diagnosed with COPD and other comorbidities, including:
- 80% reduction in hospitalizations
- 60% reduction in exacerbations
- 87% increase in patient quality of life
- NPS between 60 and 90
NuvoAir’s clinical service helps connect the dots between diagnosis and care delivery, empowering both patients and providers to take charge of their health with real-time data and timely clinical interventions. We can help health plans deliver value-based care and improve their Stars and HEDIS measures while accelerating the speed-to-care for each patient. To learn more about how NuvoAir can help diagnose and manage at-risk members in your patient population, contact our sales team today.